Overview
Vision & Mission
Vision: Ensure quality healthcare services to unreached communities and reduce morbidity
Mission:
Develop and deploy advanced technologies to increase efficiency and affordability (SDGs #9) Increase access to basic healthcare services to ensure universal healthcare coverage (SDGs #3) Design a sustainable social business model to create new employment opportunities (SDGs #1,2,5,8) Build partnerships with academia, industry, and government (SDGs #17) Organize and attend academic conferences and events (SDGs #17)
Why Unreached Community? Where is the problem?
More than half of the world’s population does not receive all the essential services they need. 100 million people are pushed into extreme poverty due to their health expenditures, forcing them to survive on just $1.90 or less a day (World Health Organization and International Bank for Reconstruction and Development, 2017). Many of them live in areas where healthcare infrastructure (clinics, doctors, etc.) is not available.
Response from Academia: Design of a Portable Health Clinic
KYUSHU UNIVERSITY and GRAMEEN COMMUNICATIONS have been jointly working since 2007 to understand the local needs and design an advanced healthcare delivery system that will be affordable by the unreached community, usable by a local healthcare worker, and financially sustainable.We prototyped a Portable Health Clinic (PHC) system, primarily considering the local infrastructure and needs of the rural communities. We developed and used advanced medical and ICT technologies to make the service systematically efficient. A social business model is proposed and examined to ensure the financial sustainability and measure the social impacts. Designing such a system requires multidisciplinary knowledge and expertise. Kyushu University teamed with experts from different disciplines: ICT experts, medical and clinical experts, public health experts, nursing experts, social science experts, data scientists, and business experts.
Portable Health Clinic: How does it work?
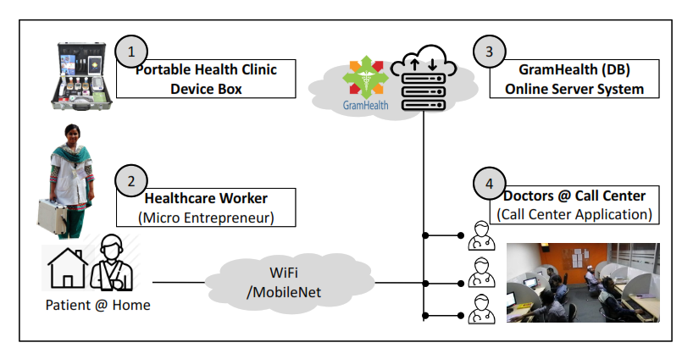
The Portable Health Clinic (PHC) system is a remote healthcare system that uses the functions of both eHealth and telemedicine systems. It comprises four major components as shown in Table 1.
Table 1: Four major components for the Portable Health Clinic System
Symbol Name Description
PHC Box
A set of sensors (thermometer, blood tester, urine tester, etc.) to measure health status, and the GramHealth Client software tool to collect healthcare data and transmit it to the server.
Healthcare worker
A licensed healthcare worker to operate the portable health clinic box, take healthcare data, and explain the results and prescriptions from the doctor.
GramHealth Server
A cloud-based software system to archive personal health records, produce statistics, and provide healthcare tips to individuals.
Telemedicine Center
A physical or virtual call center with connected licensed doctors.
A health worker visits a patient with the PHC box to measure their vital information and uploads the data with the patient’s medical history to an online server using the GramHealth Client Application installed in a smartphone or tablet PC inside the PHC box. The remote doctor accesses this data and makes a video call to the patient for further verification. Finally, the doctor creates an online prescription and enters it into the online server under each patient’s profile. The health worker accesses the system to print the prescription and instantly passes it to the patient with a detailed explanation. The entire process takes approximately 15 to 30 minutes per patient.
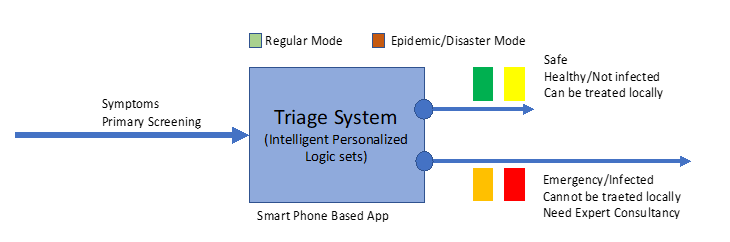
Figure 1: Triage system to identify and classify patients The PHC system introduces a triage system to classify the subjects into four categories: (i) Green (healthy), (ii) Yellow (suspicious), (iii) Orange (affected), and (iv) Red (emergent), based on a gradually increasing risk of health status. The subjects classified as Orange and Red are those primarily diagnosed as high-risk and require a doctor's consultation.
Figure 2: PHC Operational Architecture The PHC service is delivered by a trained healthcare worker and a remote doctor connected by a video conferencing system. Services include basic health checkups and regular monitoring. Basic health checkups include (a) a set of demographic questions, (b) 14 clinical measurements, and (c) consultation with a doctor for prescriptions. The 14 clinical measurements include: (1) blood pressure, (2) pulse rate, (3) body temperature, (4) blood oxygenation (SpO2), (5) arrhythmia, (6) BMI, (7) waist, hip, and waist-to-hip ratio, (8) blood glucose, (9) blood cholesterol, (10) blood hemoglobin, (11) blood uric acid, (12) blood grouping, (13) urinary sugar, and (14) urinary protein. Every patient has a health account to access their past health history and health trends. The patients and their authorized family members can access the health account. PHCs have been used in Bangladesh for purposes other than NCDs, e.g., to produce pathological reports (Tele-Pathology), provide eye-care services (Tele-EyeCare), and provide maternal and child health (MCH) care. The following types of communities have been served thus far: (a) rural unreached communities, (b) urban aging communities, (c) urban small- and medium-sized corporate communities, and (d) urban morning walker communities.
Expansion of PHC Services
Geographical Expansion of PHC The PHC concept has been introduced and partially piloted in several other countries, including India, China, Pakistan, Cambodia, Liberia, and Thailand. The PHC operation team has trained staff in India, Pakistan, Malaysia, and Thailand.
Modular Expansion of PHC The prevalence of NCDs such as diabetes mellitus and hypertension has increased to a concerning level in rural communities too. Approximately 70% of all deaths are caused by NCDs. Therefore, many NCD patients require expert consultation with further investigation. Given the need to provide further investigation and better assessment by remote doctors through telemedicine, the demand for pathological support has been noted by both patients and doctors. Consequently, the PHC system added a new module called "Tele-Pathology". Additionally, village women have fewer opportunities to see doctors in the city when necessary because they mostly stay at home and manage the household. Sometimes, local culture and religious faith act as barriers for women to see a doctor in clinics or hospitals located far away. Therefore, most village women depend on unskilled traditional quacks or rural midwives for any issues, and particularly for Ob-Gyn care. This results in many unwanted health issues and death. Therefore, PHC services found a huge need for MCH care support in the village and subsequently added a new module for MCH care. Similarly, the "Tele-Eye" care module was added in response to the need for ophthalmic care. Thus, the PHC system must gradually expand and create new modules based on the community's requirements. One such development work is now underway on "Tele-Dental" care.
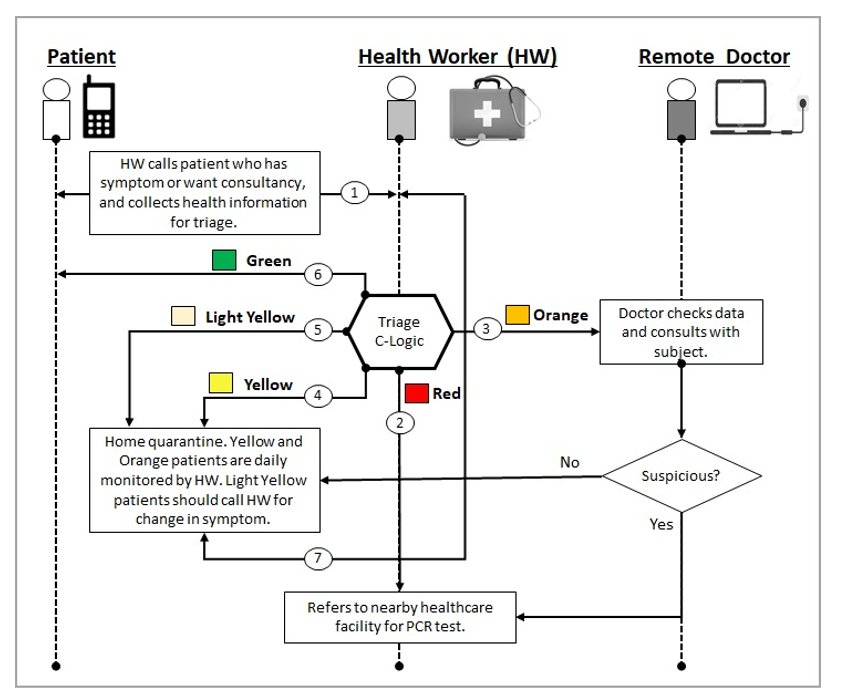
PHC for COVID-19
Considering the pandemic situation, we investigated how PHC can be made useful for our PHC registered members. We came up with a slightly modified operational step to reduce the transmission risk between the potential COVID patients and medical workers.
Figure 3: PHC operational steps during pandemic situation Figure 3 explains how PHCs will operate during COVID-19-like contexts. Unlike the conventional PHCs for NCDs, the local health worker collects the primary symptoms of a patient through a standard questionnaire. If the patient is identified as a potential patient, the PHC COVID-19 box will be sent to the patient’s home temporarily together with an operation manual so that they can check themselves under the guidance of the health worker. If a patient is identified as a potential COVID-19 carrier through this primary screening using the triage system, the patient will be immediately advised to see a nearby hospital for further investigation and follow-up as needed. Otherwise, the health worker will provide guidelines for remaining at home under quarantine. Since the patients already know the community health workers, the patients feel more comfortable and safer under their guidance. The privacy of sensitive information of patients will be protected and secured because it is required by an increasing body of legislative provisions and standards. Although the original PHC box contains various medical sensors, only COVID-19 related sensors will be used, which include the following: i) thermometer for measuring body temperature; ii) pulse oximeter for measuring blood oxygenation; iii) digital BP machine for measuring blood pressure, pulse rate, and arrhythmia; and iv) glucometer for measuring blood glucose in diabetic patients. After taking the measurements, the triage algorithm at the PHC client device classifies the patients into four categories.